|
OBESITY
SURGERY
The Center
for Obesity Surgery has been performing obesity surgery since
1983 with over 3000 cases successfully completed to date.
Our results have been excellent. There have been remarkable
advances in obesity surgery during the last few years and
we are very proud to have contributed to some of them. The
operations are very safe and effective.
There
are several types of operations done in this country to treat
obesity. They can be classified into three types: restrictive,
malabsorptive and a combination of restrictive and malabsorptive.
In 1991
the National Institutes of Health held a consensus conference
on surgery for obesity and recommended the Vertical Banded
Gastroplasty, (VBG), and the Roux-en Y Gastric Bypass (Roux-en
Y) for the treatment of severe obesity. At the Center for
Obesity Surgery the primary procedure is the Roux-en Y which
experience shows has the best results and least post-operative
complications.
The Roux-EN-Y
Gastric Bypass is a restrictive procedure combined with a
modified gastric bypass that moderately limits calorie and
nutrient absorption and may lead to altered food choices.
The Roux-en Y works by decreasing food intake, limiting the
amount of food the stomach can hold by closing off a significant
portion of the stomach and delaying the emptying of the stomach
(gastric pouch).
ROUX-EN-Y
GASTRIC BYPASS
 In
this operation the stomach is divided into two compartments
with several rows of titanium staples. The newly created stomach
pouch is measured at less than 30 cc's. The small intestine
is then divided in the proximal jejunum and the lower end
brought up and joined to the new small stomach compartment.
The pouch initially holds about 1 ounce of food and expands
to 2-3 ounces with time. The pouch's lower outlet usually
has a diameter of about 1/2-inch. The small outlet delays
the emptying of food from the pouch and causes a feeling of
fullness. After an operation, the person usually can eat only
5 to 10 bites of food before feeling full. With time, the
capacity may increase to half to a whole cup of food that
may be consumed without discomfort or nausea. Food has to
be well chewed. For most people, the ability to eat a large
amount of food at one time is lost, and some of the food consumed
will not be absorbed due to the bypass segment of the operation. In
this operation the stomach is divided into two compartments
with several rows of titanium staples. The newly created stomach
pouch is measured at less than 30 cc's. The small intestine
is then divided in the proximal jejunum and the lower end
brought up and joined to the new small stomach compartment.
The pouch initially holds about 1 ounce of food and expands
to 2-3 ounces with time. The pouch's lower outlet usually
has a diameter of about 1/2-inch. The small outlet delays
the emptying of food from the pouch and causes a feeling of
fullness. After an operation, the person usually can eat only
5 to 10 bites of food before feeling full. With time, the
capacity may increase to half to a whole cup of food that
may be consumed without discomfort or nausea. Food has to
be well chewed. For most people, the ability to eat a large
amount of food at one time is lost, and some of the food consumed
will not be absorbed due to the bypass segment of the operation.
They are
more interested in lighter and healthier food. Most patients
report that their tastes change after surgery. Many patients
experience the "dumping syndrome" in which foods; usually
those high in fat and/or sugar are not well tolerated. In
the dumping syndrome stomach contents move too rapidly through
the small intestine. Symptoms include nausea, weakness, sweating,
faintness, and, occasionally, diarrhea after eating these
foods. Patients find that this negative incentive helps them
to eliminate high caloric foods and sweets from their diets.
At the
Center for Obesity Surgery we recommend the Proximal Roux-En-Y
gastric Bypass and we do it through a small midline incision
(mini-lap), 4-5 inches, and the skin is closed with sutures
under the skin (plastic surgery closure).
In our
opinion, based on 21 years of experience this operation optimizes
safety and effectiveness of the proximal Roux-En-Y Gastric
Bypass through:
- Excellent
cosmetic result (small incision)
- Short
operating time (Average 1.5 hours)
- Short
hospital stay (Average 2 days)
- Less
pain (Use of narcotics 2-3 days)
- Fast
recovery (Back to work in 10-12 days)
- Safety
(less complication rate)
ADVANTAGES
- Greatly
controls food intake
- Dumping
syndrome - eliminates high calorie foods and sweets from
diet
- Decrease
appetite
- Limit
Caloric Absorption
- Reversible
in an emergency - though this procedure should be thought
of as permanent
DISADVANTAGES
- Staple
line failure (Less than 5%)
- Narrowing/blockage
of the stomach (Less than 1%)
- Vomiting
if food is not properly chewed or if food is eaten too quickly
Other
less common procedures include
ADJUSTABLE
GASTRIC BANDING (AGB)
In this
procedure, a silicone band is placed around the upper part
of the stomach to create a small stomach pouch, which can
hold only a small amount of food. The lower, larger part of
the stomach is below the band. These two parts are connected
by a small outlet created by the band. Food will pass from
the upper stomach pouch to the lower part more slowly, and
one will feel full longer. The diameter of the band outlet
is adjustable.
ADVANTAGES
- Simple
- Short
recovery period
- Major
complication rate is low
- No
altering of the natural anatomy
DISADVANTAGES
- Patient
non-compliance causes high failure rate
- Complications
include :
- Balloon
leakage
- Band
erosion/migration
- Deep
infection
- Identifying
patients who will not "eat through" the operation
is difficult
- Weight
loss is 15-25% less than Roux-En-Y Gastric Bypass
 VERTICAL
BANDED GASTROPLASTY (VGB) VERTICAL
BANDED GASTROPLASTY (VGB)
This,
along with the RNY, is one of the two major types of operations
recognized by the NIH for the treatment of clinically severe
obesity. It is a purely restrictive procedure with no malabsorptive
effect. The goal of this procedure is to severely restrict
the patient's capacity to eat certain foods.
ADVANTAGES
- Completely
reversible
- No
dumping syndrome
- No
nutritional deficiencies
DISADVANTAGES
- Needs
strict patient compliance to diet
- No
malabsorbtion
- Vomiting
if food is not properly chewed or if food is eaten too quickly
- Conversion
to RYGB is common
- Weight
loss is 15-20% less than the Roux-En-Y Gastric Bypass
 DUODENAL
SWITCH - DS DUODENAL
SWITCH - DS
There
is a significant malabsorptive component that acts to maintain
weight loss long term. The patient must be closely monitored
to guard against severe nutritional deficiencies. This procedure,
unlike the Bilio Pancreatic Diversion, keeps the pyloric valve
intact. That is the main difference between the BPD and the
DS.
ADVANTAGES
- More
"normal" absorption of many nutrients than with
BPD, including calcium, iron and vitamin B12
- Better
eating quality when compared to other WLS procedures.
- Eliminates
or greatly minimizes most negative side effects of the original
BPD
- Essentially
eliminates stomal ulcer and dumping syndrome
DISADVANTAGES
- Greater
chance of chronic diarrhea
- Significant
malabsorptive component
- More
foul smelling stools and flatus but less than with the BPD
alone
- High
risk of nutritional deficiencies.
 BILIOPANCREATIC
DIVERSION (SCOPINARO PROCEDURE) BPD BILIOPANCREATIC
DIVERSION (SCOPINARO PROCEDURE) BPD
This
procedure is less food restrictive than the RNY. The stomach
capacity is 8-10 ounces compared with RNY of around an ounce.
There is a significant malabsorptive component, which acts
to maintain weight loss long term. The patient must be closely
monitored to guard against severe nutritional deficiencies.
ADVANTAGES
- Significant
malabsorptive component
- Better
chance of sustained weight loss
- Ability
to eat larger quantities of food and still lose weight
DISADVANTAGES
- Greater
chance of chronic diarrhea, stomal ulcers, more foul smelling
stools and flatus
- Higher
risk of nutritional deficiencies
- Higher
chance of micronutrient deficiencies such as vitamins and
calcium
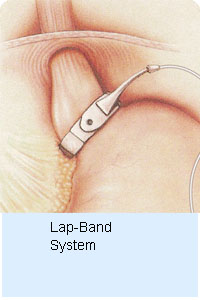 THE LAP-BAND SYSTEM THE LAP-BAND SYSTEM
A silicone band is placed around the upper part of the stomach. From this a small pouch is created making the stomach hold less food and including the feeling of satiety.
ADVANTAGES
- 10 x safer than Gastric Bypass
- Adjustable - customized per patient
- Least invasive option
- No stomach stapling, cutting or interstinal rerouting
- Reversible
- Lowest operative complication rate - no leaks
- Low malnutrition risk
- Satiety-including procedure
- OR time = 1 hour or less
- Overnight hospital stay in most cases
RISKS
As with
any major abdominal surgery there are potential risks. These
risks can be further complicated in operations on severely
obese patients. It is important that you consider these potential
risks, and discuss them with Dr. Afram and your own physician,
when deciding whether to have surgery. Potential surgical
risks include possible respiratory problems, infections, bleeding,
bowel obstruction, leakage of the bowel connections, and obstruction
of the stomach outlet. After performing over 3000 gastric
bypass operations, Dr. Afram and his team have developed successful
strategies for minimizing any potential risks.
POTENTIAL
SIDE EFFECTS OF THE SURGERY
Due to
the physical changes caused by the gastric bypass surgery,
there are potential side effects that result from the surgery
and your new way of eating. Due to restricted eating, there
is a potential for deficiencies in protein, as well as certain
vitamins and minerals. Use of an over-the-counter multivitamin,
fortified with iron and calcium, and other nutritional supplements,
determined on an individual basis, can help mitigate this
risk.
Some
patients experience nausea, food intolerance, changed bowel
habits, transient hair loss, and loss of muscle mass. It is
important to note that not all patients experience these side
effects and these side effects are usually transitory. If
you experience any of these post-operative side effects, Dr.
Afram and the nutritionist are available for immediate consultation.
Gall bladder
disease is a potential side effect due to the rapid weight
loss most patients experience after the surgery. To minimize
this risk Dr. Afram may prescribe medication, taken regularly
for several months after surgery.
A
word about pregnancy.
Infertility
can be a significant co-morbidity for severely obese women.
Many obese women experience irregular or non-existent menstrual
cycles. Surgery for obesity often corrects these problems.
Due to the increased nutritional needs of pregnancy, we recommend
that patients not get pregnant for at least one to two years
after surgery, when the initial rapid weight loss subsides.
Patients should discuss birth control methods with their primary
care physician or obstetrician/gynecologist. After the initial
year, pregnancy is safe and many patients, who had suffered
from infertility prior to surgery, have delivered healthy
babies.
RESULTS
Most
of our patients are very satisfied with the results of their
operation. Overwhelmingly, patients have found that they lose
50 to 90 percent of their excess weight, and maintain that
weight loss long-term.
Maximum
effectiveness depends on the level of patient participation
in the behavioral modification and nutritional programs, as
well as an increase in physical activities and exercise on
a regular basis. Other factors, such as age, sex, and initial
weight at the time of surgery should also be considered. Weight
loss surgery is not a magic bullet. It is, however, a powerful
tool that has successfully helped many people achieve and
maintain permanent weight loss. Your active participation
in, and commitment to, the life style changes, exercise, and
eating habits that weight loss surgery requires is a necessary
component to your ultimate success.
Most medical
diseases are improved or cured. Obesity related diseases are
improved dramatically.
- High
Blood Pressure can be often alleviated or eliminated
by weight loss surgery
- High
Blood Cholesterol in 80% of the patients can be alleviated
or eliminated and in as little as 2-3 months post-operatively
- Heart
Disease in obese individuals is certainly more likely
to be experienced when compared to persons who are of average
weight and adhere to a strict diet and exercise regimen.
There is no hard and fast statistical data to definitively
prove that weight loss surgery reduces the risk of cardiovascular
disease, however, common sense would dictate that if we
can significantly reduce many of the co-morbidities that
we experienced as someone that is obese, we can likewise
that our health may be much improved if not totally restored.
- Diabetes
Mellitus can be cured or tremendously improved. Complications
can be controlled based on many post gastric bypass studies.
- Abnormal
Glucose Tolerance, or "Borderline Diabetes"
is even more likely reversed by Gastric Bypass. Since this
condition becomes diabetes in many cases, the operation
can frequently prevent diabetes as well
- Asthma
sufferers may find that they have fewer and less severe
attacks, or sometimes none at all. When asthma is associated
with gastroesophageal reflux disease, it is particularly
benefited by gastric bypass.
- Sleep
Apnea Syndrome sufferers can receive dramatic effects
and many within a year or so of surgery find their symptoms
were completely gone and they ever stopped snoring completely!
- Gastroesophageal
Reflux Disease can be greatly relieved of all symptoms
within as little as a few days of surgery
- Gallbladder
Disease can be surgically handled at the time of weight
loss surgery if your doctor has cause to believe that gallstones
are present.
- Stress
Urinary Incontinence responds dramatically to weight
loss, usually by becoming completely controlled. A person
who is still troubled by incontinence can choose to have
specific corrective surgery later, with much greater chance
of a successful outcome, with a reduced body weight.
- Low
Back Pain and Degererative Disk Disease, and Degenerative
Joint Disease can be considerable relieved with weight
loss, and greater comfort may be experienced even after
as few as 30 pounds are lost.
- Major
improvement in the quality of life and improvement in self-esteem
and self-confidence.
|
![]()


 In
this operation the stomach is divided into two compartments
with several rows of titanium staples. The newly created stomach
pouch is measured at less than 30 cc's. The small intestine
is then divided in the proximal jejunum and the lower end
brought up and joined to the new small stomach compartment.
The pouch initially holds about 1 ounce of food and expands
to 2-3 ounces with time. The pouch's lower outlet usually
has a diameter of about 1/2-inch. The small outlet delays
the emptying of food from the pouch and causes a feeling of
fullness. After an operation, the person usually can eat only
5 to 10 bites of food before feeling full. With time, the
capacity may increase to half to a whole cup of food that
may be consumed without discomfort or nausea. Food has to
be well chewed. For most people, the ability to eat a large
amount of food at one time is lost, and some of the food consumed
will not be absorbed due to the bypass segment of the operation.
In
this operation the stomach is divided into two compartments
with several rows of titanium staples. The newly created stomach
pouch is measured at less than 30 cc's. The small intestine
is then divided in the proximal jejunum and the lower end
brought up and joined to the new small stomach compartment.
The pouch initially holds about 1 ounce of food and expands
to 2-3 ounces with time. The pouch's lower outlet usually
has a diameter of about 1/2-inch. The small outlet delays
the emptying of food from the pouch and causes a feeling of
fullness. After an operation, the person usually can eat only
5 to 10 bites of food before feeling full. With time, the
capacity may increase to half to a whole cup of food that
may be consumed without discomfort or nausea. Food has to
be well chewed. For most people, the ability to eat a large
amount of food at one time is lost, and some of the food consumed
will not be absorbed due to the bypass segment of the operation.
 VERTICAL
BANDED GASTROPLASTY (VGB)
VERTICAL
BANDED GASTROPLASTY (VGB) DUODENAL
SWITCH - DS
DUODENAL
SWITCH - DS BILIOPANCREATIC
DIVERSION (SCOPINARO PROCEDURE) BPD
BILIOPANCREATIC
DIVERSION (SCOPINARO PROCEDURE) BPD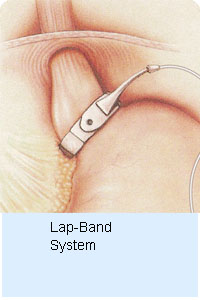 THE LAP-BAND SYSTEM
THE LAP-BAND SYSTEM